-
 Thanh toán đa dạng, linh hoạtChuyển khoản ngân hàng, thanh toán tại nhà...
Thanh toán đa dạng, linh hoạtChuyển khoản ngân hàng, thanh toán tại nhà... -
 Miễn Phí vận chuyển 53 tỉnh thànhMiễn phí vận chuyển đối với đơn hàng trên 1 triệu
Miễn Phí vận chuyển 53 tỉnh thànhMiễn phí vận chuyển đối với đơn hàng trên 1 triệu -
 Yên Tâm mua sắmHoàn tiền trong vòng 7 ngày...
Yên Tâm mua sắmHoàn tiền trong vòng 7 ngày...
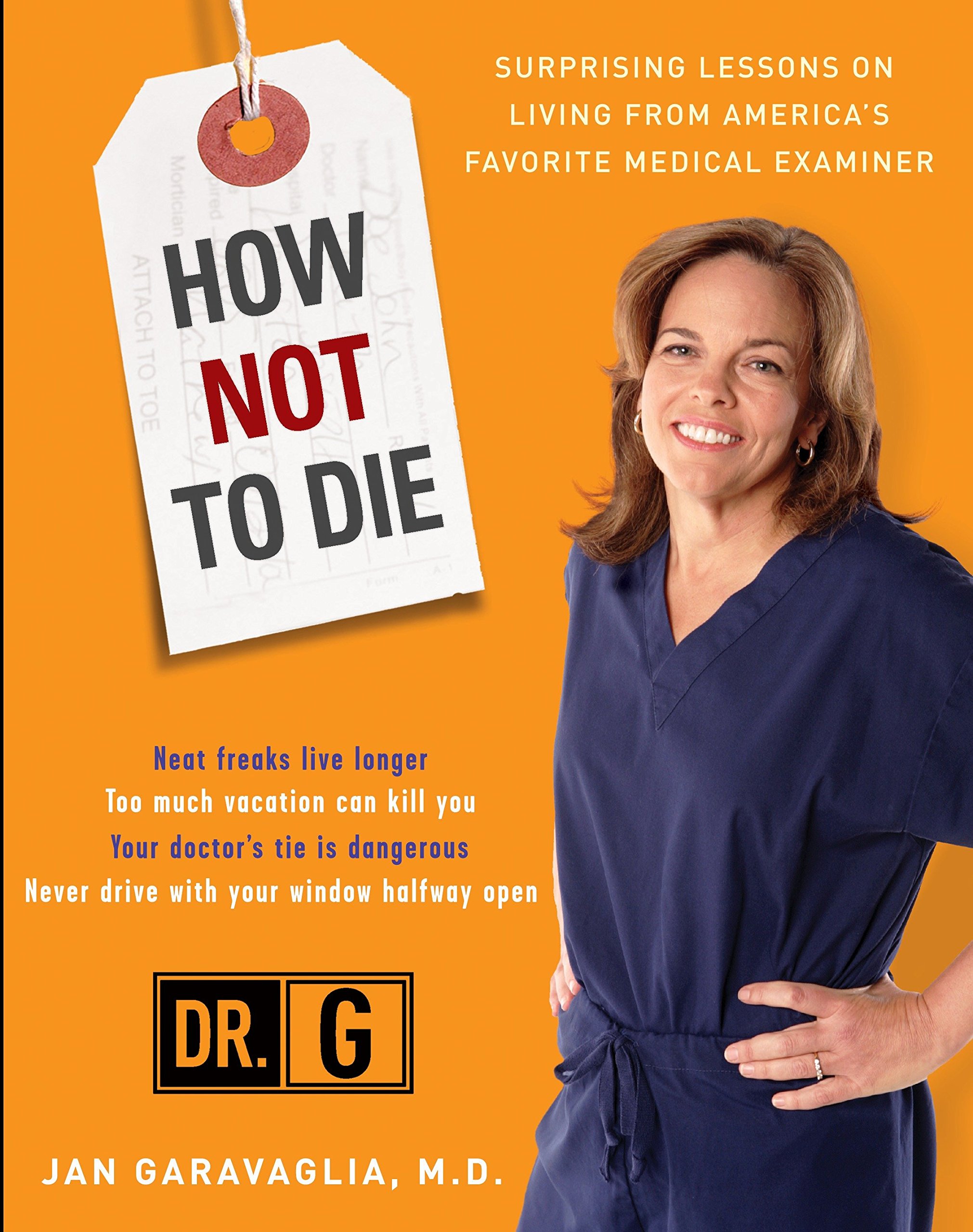
How Not to Die: Surprising Lessons from America's Favorite Medical Examiner
-

- Mã sản phẩm: 0307409155
- (524 nhận xét)

- Publisher:Harmony; 1st edition (September 15, 2009)
- Language:English
- Paperback:288 pages
- ISBN-10:0307409155
- ISBN-13:978-0307409157
- Item Weight:12.6 ounces
- Dimensions:7.45 x 0.6 x 9.06 inches
- Best Sellers Rank:#89,988 in Books (See Top 100 in Books) #45 in Safety & First Aid (Books) #115 in Longevity #198 in Medical Professional Biographies
- Customer Reviews:4.6 out of 5 stars 525Reviews
Mô tả sản phẩm
Product Description
WHEN THIS DOCTOR TALKS, YOU SHOULD LISTEN.
Thousands of people make an early exit each year and arrive on medical examiner Jan Garavaglia’s table. What is particularly sad about this is that many of these deaths could easily have been prevented. Although Dr. Garavaglia, or Dr. G, as she’s known to many, could not tell these individuals how to avoid their fates, we can benefit from her experience and profound insight into the choices we make each day.
In How Not to Die, Dr. G acts as a medical detective to identify the often-unintentional ways we harm our bodies, then shows us how to use that information to live better and smarter. She provides startling tips on how to make wise choices so that we don’t have to see her, or someone like her, for a good, long time.
• In “Highway to the Morgue,” we learn the one commonsense safety tip that can prevent deadly accidents—and the reason you should never drive with the windows half open
• “Code Blue” teaches us how to increase our chances of leaving the hospital alive—and how to insist that everyone caring for you practice the easiest hygiene method around
• “Everyday Dangers” informs us why neat freaks live longer—and the best ways to stay safe in a car during a lightning storm
Using anecdotes from her cases and a liberal dose of humor, Dr. G gives us her prescription for living a healthier, better, longer life—and unlike many doctors’ orders, this one is surprisingly easy to follow.
About the Author
JAN GARAVAGLIA, M.D., is the chief examiner for the District 9 Medical Examiner’s Office in Florida, presiding over 1,100 autopsies a year. She is also the host of Discovery Health channel’s top-rated series, Dr. G: Medical Examiner.
Excerpt. © Reprinted by permission. All rights reserved.
ONE
Doctor Dread
Taking It on the Jaw
I followed the infection underneath his breastbone like a trail of bread crumbs all the way up to his jaw. The trail teemed with pus, the army of white blood cells that had marched through the walls of blood vessels to fight invading microorganisms. I had never seen anything like it before. Bacteria had waged a protracted war with his body's immune system-and won. I wondered how fifty-year-old Victor Baca could have developed such a virulent infection.
Ten days earlier, Victor had been in perfect health. Then he started complaining of back and shoulder pain and a sore throat. The symptoms kept him in bed and unable to go to work. Even so, he didn't seek medical attention. But as the pain worsened, Victor realized something was terribly wrong, and he called 911. The dispatcher alerted an ambulance. Paramedics arrived, found him critically ill, and went to work immediately. Despite their aggressive intervention, including cardiopulmonary resuscitation (CPR), Victor slipped away, causes unknown.
As I often do in cases involving unusual infections, after the autopsy I consulted Dr. Mark Wallace, an infectious disease specialist and an internal medicine physician, who also happens to be my husband. An infectious disease specialist tracks down bacteria and viruses, decodes their defenses and their weaknesses, and figures out what will kill them. Mark believed-and I concurred-that all the evidence proved that a bacterial infection had originated in Victor's mouth, shockingly, from the most ordinary of health problems: a common dental infection. This infection probably migrated from a decayed tooth into the surrounding bone and tissue in his jaw and caused an abscess, a cavity containing pus surrounded by inflamed tissue. Many of us have probably had an abscess at one time or another. They can show up externally (in the gums or in a hair follicle) or internally (in an organ), and some types are more severe than others.
Once a pocket of pus breaks through the thin bone surrounding the tooth sockets, bacteria can spread through the tissue planes of the neck and into the chest. By the time Victor sought medical attention, bacteria had likely reached his bloodstream and caused multisystem organ failure. This infection was the source of all his pain-and the cause of his death. Before penicillin was discovered in 1928, bacterial infections like Victor's were the leading cause of death in the United States. Today, due to widespread use of antibiotics, head and neck infections rarely kill, unless you have no access to, or reject, basic medical or dental care. For some unknown reason, Victor decided not to see a doctor, even as the unchecked infection spread to his chest and the pain became excruciating. What began as a run-of-the-mill oral infection became a fight for survival. Eventually, Victor's organs ceased functioning, and he died. The tragedy was compounded by the fact that Victor's death could easily have been prevented. A routine course of antibiotics provided in a timely manner would have stopped the infection in its tracks.
Checked Out
As with the case of Victor Baca, I've seen firsthand the terrible complications that can arise when people don't go to the doctor, ignore a physician's advice, or decide to take medical matters into their own hands. Another example from my case files is that of Kim Atani, age forty-eight. She was a woman who could have lived a long, normal life had she received proper medical care. Kim, who was blind, and her husband, Simon, were living in their Orlando home when Simon found her collapsed on the bedroom floor. He called 911, and Kim was rushed to the hospital, where she later died. Her body was sent to my morgue to be autopsied.
Some of the most important information any physician-forensic pathologists included-can have is a medical history. But Kim arrived at the morgue without any medical records. I had to rely solely on observation to figure out why she died. Clearly, something terrible had been happening. Her teeth were fractured at the gum line. She was also covered with bedsores, oozing craterlike wounds that can become seriously infected. Medically known as "decubitus ulcers," bedsores develop quickly as tissue dies when blood flow is impaired by the continuous pressure of body weight on the soft tissues sandwiched between bone and a firm surface. There was also gangrene, or dead tissue, which appeared as large, black, shriveled areas across her left foot. Gangrene is caused by progressive loss of blood to an area, and there are two types: wet and dry. Both are caused by poor blood flow, but in wet gangrene, the tissue is also infected with bacteria. Kim had wet gangrene. Gangrene is often associated with advanced cases of diabetes.
I dissected Kim's wet gangrene and discovered that the infection had burrowed down to her bone. If discovered in time, a limb so acutely diseased would have been amputated to prevent the spread of a life-threatening infection. With my scalpel, I made the standard Y incision, a deep cut from shoulder to shoulder across the chest, followed by a straight line down to the pubic bone. I then opened the torso like you'd open a jacket or sport coat. Ribs were cut so I could gain access to the organs, which are removed, weighed, and dissected during the autopsy. After opening her up, I could see that her body harbored several other possible killers. Her kidneys and liver were damaged, and her coronary arteries were more than 95 percent blocked. These findings were pieces of the puzzle that, along with her blindness, periodontal disease, and gangrene, began to fit a pattern. It appeared to me that Kim Atani had been suffering from long-standing untreated diabetes.
Diabetes is a metabolic disorder. Its hallmark is a failure to metabolize glucose, or blood sugar, carried by the bloodstream to fuel every part of the body. The failure is caused by problems with the hormone insulin. Either the body doesn't make any (or enough) insulin, or cells don't respond to insulin properly. In either situation, glucose is unable to enter cells. It starts amassing in the bloodstream, where it can reach concentrations over ten times the normal level. Over time, elevated glucose causes widespread organ damage, like that which I observed in Kim Atani. To confirm that Kim had diabetes, I would need to know her blood sugar levels. Testing for blood sugar is easy to do when you're living-blood is drawn and checked for its glucose concentration-but it's more complicated when you're dead. After you die, your blood sugar begins to drop continuously toward zero. I can't even test for glucose levels in the blood because the blood breaks down right after death and interferes with testing. But I can test for glucose by using eye fluid drawn into a syringe-a procedure that can make you shudder if you've never seen it before. Each adult human eye contains about one-fifth of a teaspoon of jellylike fluid called vitreous humor. This fluid is very reliable for testing because it is isolated and protected, and therefore less subject to contamination or cell breakdown. I collected eye fluid from Kim's eyes and sent it to our toxicology lab. Glucose levels in the eye decrease after death, too, so a finding of elevated glucose would strongly indicate diabetes. Sure enough, when the toxicology report came back, it revealed that Kim's eye-fluid glucose was 378-massively elevated for a postmortem level.
Once I put all the facts of the case together and reviewed her tissues under a microscope, it was clear to me that over time, elevated glucose had caused widespread organ disease. It not only left Kim blind but it also caused a loss of sensation in her extremities and impaired her blood flow. Gangrene set in and allowed a deadly infection to take hold. The infection invaded her bloodstream, causing sepsis-an often fatal condition. Sepsis takes its name from the Greek word meaning "to putrefy." Known for generations as "blood poisoning," it generally means bacteria have breached the natural barriers of the skin and organs to enter the bloodstream. Once there, they produce an overwhelming infection, the biological equivalent of tossing a grenade into your body. Blood pressure drops, vessels leak, and the lungs and kidneys fail. The result can be septic shock so severe that no amount of intravenous fluid or medication can reverse the condition. This is what happened to Kim Atani.
Normally, a case like this would be closed, but I had to get to the bottom of why she had not sought medical care. Was it a case of negligence on the part of her husband, Simon? Could his inaction have contributed to her untimely death? If it was found that he had acted negligently, charges could be brought against him. I called Simon and told him that his wife had had diabetes. He was in denial about it, but more from ignorance about the disease than anything else. I pointedly asked why she didn't seek medical care and why he didn't seek medical care for her. He told me that his wife had had some bad experiences with doctors, that she refused to see one, and that she hated the medical establishment. There was nothing he could do to get Kim to see a doctor, and so he vowed that he would do what he could to take care of her. In the end, and after confirming her fear of the medical system, I believed him. He was sincere and really cared about his wife.
Many people make choices that ultimately lead to their demise, and at autopsy, my findings reflect this. As a medical examiner, I'm one of the few people given permission to look behind the curtain of someone's life, and what I observe is often senseless and tragic. I don't judge how people live, but I will say this: Not going to the doctor when you have a major health issue is your decision, but missing needed care might mean I'll be the doctor you'll eventually visit. Kim Atani and Victor Baca suffered not only from deadly but treatable illnesses; they also may have suffered from latrophobia or odontophobia. These are medical terms that describe a fear of doctors or dentists, respectively, in which people put off getting medical attention, making excuse after excuse, until sometimes it's too late.
Why do we fear doctors? I think one of the big reasons is that we're filled with dread that some serious problem might be found and we're afraid of hearing bad news. It's scary to be a patient. It's even scary for me to be a patient! Though we like to think we'll live forever, we're all here temporarily. Seeing a doctor brings us face-to-face with our own mortality.
There are other reasons we avoid seeing a doctor. Maybe you don't think your symptoms are important. Maybe you're concerned about wasting a doctor's time. Or maybe you don't want to spend the money because you're uninsured. I can't tell you how many people I've autopsied because they didn't want to incur a medical bill.
Or maybe you're a man. Men in this country are much less likely to see a doctor than women are. Their reluctance may be one reason why the life expectancy of men is eight years shorter than that of women. Men repress pain, ignore symptoms, and deny sickness, in part to demonstrate their manhood. Society conditions men to "tough out" illness. They don't want to feel like wimps or go to the doctor for nothing. If a man does see a doctor, it's often because a woman in his life has made him go.
How Not to Die from Latrophobia or Odontophobia
No one likes to get sick. It means that you can't do the things you enjoy or the things you live for. When you're sick, you don't feel like doing much of anything, except lying in bed. You might get better on your own, but then again, you might not. If you stay sick long enough, sooner or later you'll have to go to the doctor, whether you want to or not.
Wanted: A Great Doctor
If you're afraid of doctors, one of the best ways to get over your fear is to be under the care of one you like and trust. To find that kind of doctor takes a bit of sleuthing. Here's what I do: I look for a doctor who is geographically convenient, and I won't go to any doctor who is not board certified in his or her specialty or subspecialty. Board certification means that a doctor has had extra training after medical school and internship in an approved training program to become an expert in a field of medicine such as family practice, internal medicine, or gynecology, then has passed a rigorous qualifying examination ("the boards").
Personality is important to me, too, so I ask around to get a feel for what a doctor is like. Nurses are a great resource, since they're the ones who work with doctors day to day and see how they treat patients. I also ask friends, family, coworkers, and colleagues. Another good source is the website of the American Medical Association (www.ama-assn.org) with its DoctorFinder link. It gives you basic professional information on virtually every licensed physician in the United States. Of course, if you belong to a managed health-care plan, your choices are limited to doctors who are a part of that plan.
I also want a doctor who treats me with respect and doesn't sugarcoat things. What you need most is good communication. You end up telling a doctor a lot of intimate details about your life. If you feel uncomfortable doing so, that's your signal to find another one. Here are ten questions to ask when choosing a new doctor:
1. Are you board certified in your specialty?
2. What type of health insurance do you take? (If applicable, find out if the doctor accepts Medicare.)
3. How frequently do you see patients who have the same health problems as I have?
4. Do you refer patients to other doctors for special problems as needed?
5. Will I need to go to another location for blood tests or are lab tests done in your office?
6. If yours is a group practice, who are the other doctors and what are their specialties?
7. Who sees patients for you if you are out of town or not available?
8. Which hospitals do you use? Will you take care of me in the hospital if I'm admitted? If not, who will? (Make sure you're comfortable being treated at one of these institutions, should the need arise.)
9. How far in advance do I need to make an appointment to see you?
10. If I've got a problem (say a drug reaction or a treatment side effect) can I speak to you or your covering physician within a reasonable time frame?
- Mua astaxanthin uống có tốt không? Mua ở đâu? 29/10/2018
- Saffron (nhụy hoa nghệ tây) uống như thế nào cho hợp lý? 29/09/2018
- Saffron (nghệ tây) làm đẹp như thế nào? 28/09/2018
- Giải đáp những thắc mắc về viên uống sinh lý Fuji Sumo 14/09/2018
- Công dụng tuyệt vời từ tinh chất tỏi với sức khỏe 12/09/2018
- Mua collagen 82X chính hãng ở đâu? 26/07/2018
- NueGlow mua ở đâu giá chính hãng bao nhiêu? 04/07/2018
- Fucoidan Chính hãng Nhật Bản giá bao nhiêu? 18/05/2018
- Top 5 loại thuốc trị sẹo tốt nhất, hiệu quả với cả sẹo lâu năm 20/03/2018
- Footer chi tiết bài viết 09/03/2018
- Mã vạch không thể phân biệt hàng chính hãng hay hàng giả 10/05/2023
- Thuốc trắng da Ivory Caps chính hãng giá bao nhiêu? Mua ở đâu? 08/12/2022
- Nên thoa kem trắng da body vào lúc nào để đạt hiệu quả cao? 07/12/2022
- Tiêm trắng da toàn thân giá bao nhiêu? Có an toàn không? 06/12/2022
- Top 3 kem dưỡng trắng da được ưa chuộng nhất hiện nay 05/12/2022
- Uống vitamin C có trắng da không? Nên uống như thế nào? 03/12/2022
- [email protected]
- Hotline: 0909977247
- Hotline: 0908897041
- 8h - 17h Từ Thứ 2 - Thứ 7
Đăng ký nhận thông tin qua email để nhận được hàng triệu ưu đãi từ Muathuoctot.com
Tạp chí sức khỏe làm đẹp, Kem chống nắng nào tốt nhất hiện nay Thuoc giam can an toan hiện nay, thuoc collagen, thuoc Dong trung ha thao , thuoc giam can LIC, thuoc shark cartilage thuoc collagen youtheory dau ca omega 3 tot nhat, dong trung ha thao aloha cua my, kem tri seo hieu qua, C ollagen shiseido enriched, và collagen shiseido dạng viên , Collagen de happy ngăn chặn quá trình lão hóa, mua hang tren thuoc virility pills vp-rx tri roi loan cuong duong, vitamin e 400, dieu tri bang thuoc fucoidan, kem chống nhăn vùng mắt, dịch vụ giao hang nhanh nội thành, crest 3d white, fine pure collagen, nên mua collagen shiseido ở đâu, làm sáng mắt, dịch vụ cho thue kho lẻ tại tphcm, thực phẩm tăng cường sinh lý nam, thuoc prenatal bổ sung dinh dưỡng, kem đánh răng crest 3d white, hỗ trợ điều trị tim mạch, thuốc trắng da hiệu quả giúp phục hồi da. thuốc mọc tóc biotin





















 KHUYẾN MÃI LỚN
KHUYẾN MÃI LỚN Hỗ Trợ Xương Khớp
Hỗ Trợ Xương Khớp Bổ Não & Tăng cường Trí Nhớ
Bổ Não & Tăng cường Trí Nhớ Bổ Sung Collagen & Làm Đẹp
Bổ Sung Collagen & Làm Đẹp Bổ Thận, Mát Gan & Giải Độc
Bổ Thận, Mát Gan & Giải Độc Chăm Sóc Sức khỏe Nam Giới
Chăm Sóc Sức khỏe Nam Giới Chăm Sóc Sức khỏe Nữ Giới
Chăm Sóc Sức khỏe Nữ Giới Chăm sóc Sức khỏe Trẻ Em
Chăm sóc Sức khỏe Trẻ Em Thực Phẩm Giảm Cân, Ăn Kiêng
Thực Phẩm Giảm Cân, Ăn Kiêng Bổ Sung Vitamin & Khoáng Chất
Bổ Sung Vitamin & Khoáng Chất Bổ Tim Mạch, Huyết Áp & Mỡ Máu
Bổ Tim Mạch, Huyết Áp & Mỡ Máu Bổ Mắt & Tăng cường Thị lực
Bổ Mắt & Tăng cường Thị lực Điều Trị Tai Mũi Họng
Điều Trị Tai Mũi Họng Sức Khỏe Hệ Tiêu hóa
Sức Khỏe Hệ Tiêu hóa Chăm Sóc Răng Miệng
Chăm Sóc Răng Miệng Chống Oxy Hóa & Tảo Biển.
Chống Oxy Hóa & Tảo Biển.