-
 Thanh toán đa dạng, linh hoạtChuyển khoản ngân hàng, thanh toán tại nhà...
Thanh toán đa dạng, linh hoạtChuyển khoản ngân hàng, thanh toán tại nhà... -
 Miễn Phí vận chuyển 53 tỉnh thànhMiễn phí vận chuyển đối với đơn hàng trên 1 triệu
Miễn Phí vận chuyển 53 tỉnh thànhMiễn phí vận chuyển đối với đơn hàng trên 1 triệu -
 Yên Tâm mua sắmHoàn tiền trong vòng 7 ngày...
Yên Tâm mua sắmHoàn tiền trong vòng 7 ngày...
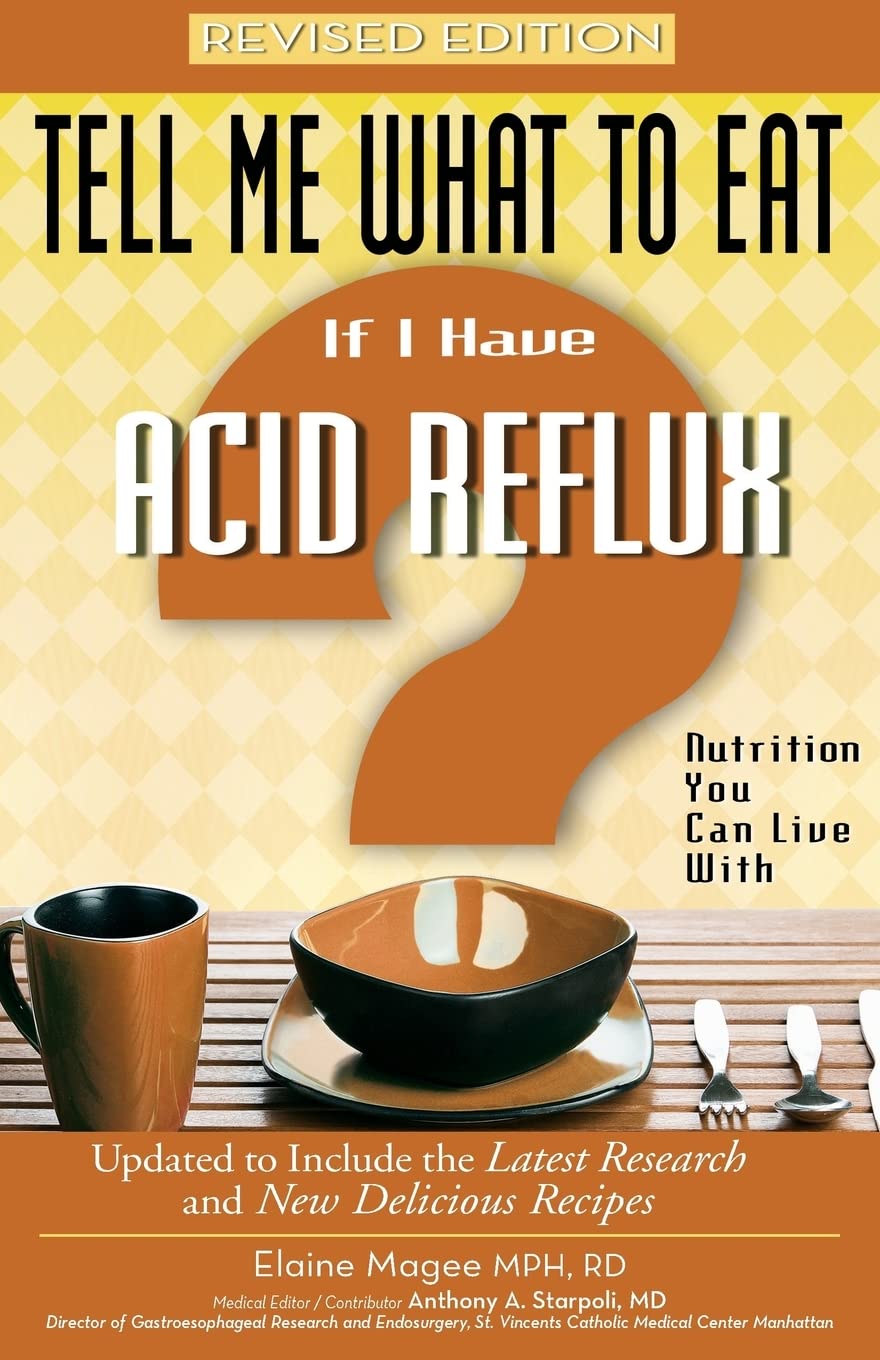
Tell Me What to Eat if I Have Acid Reflux, Revised Edition: Nutrition You Can Live With (Tell Me What to Eat series)
-

- Mã sản phẩm: 1601630190
- (159 nhận xét)

- ASIN:1601630190
- Publisher:Weiser; First Edition, Revised (October 15, 2008)
- Language:English
- Paperback:192 pages
- ISBN-10:9781601630193
- ISBN-13:978-1601630193
- Item Weight:7.5 ounces
- Dimensions:5.5 x 0.5 x 8.25 inches
- Best Sellers Rank:#1,167,487 in Books (See Top 100 in Books) #389 in Gastroenterology (Books) #802 in Abdominal Disorders & Diseases (Books) #7,012 in Other Diet Books
- Customer Reviews:4.1 out of 5 stars 159Reviews
Mô tả sản phẩm
About the Author
Elaine Magee, MPH, RD, is fondly known through her national column and on WebMD.com as "The Recipe Doctor." She is the author of 25 books on nutrition and healthy cooking, including the revolutionary Food Synergy, as well as other best-selling titles in the 'Tell Me What to Eat' series, covering type-2 diabetes, acid reflux, irritable bowel syndrome, and other important health issues. She frequently appears on television and radio shows across the country and resides in Northern California with her husband and two teenage daughters.
Product Description
Heartburn isn--t just a minor inconvenience--it is very painful and can inhibit your sleep, affect your work, and make you feel miserable. Of course, if you are one of the 60 million Americans who get heartburn at least once a month, you already know this.
Heartburn happens when the lining of the esophagus comes in contact with too much stomach juice, which can produce a burning pain and injure the esophagus. There is a valve that connects the end of the esophagus with the stomach, which normally functions to keep the stomach acid where it belongs--in the stomach. But in people with frequent heartburn, this valve relaxes too frequently, allowing the stomach acid to splash up into the esophagus.
Tell Me What to Eat If I Have Acid Reflux begins with an overview of acid reflux. Readers get a detailed yet completely understandable explanation of how and why this condition begins--an explanation that is based on the latest medical information. The majority of the book is dedicated to all the ways that diet and lifestyle can bring relief and decrease heartburn, including an entire section with specific tips and recipes to help you during the worst times of the year for heartburn sufferers--the holiday season.
Tell Me What to Eat If I Have Acid Reflux offers dozens of healthful, practical, tasty recipe options for foods you never thought you could enjoy again, plus heartburn-savvy tips on navigating the supermarket, cooking in your kitchen, and eating out.
Excerpt. © Reprinted by permission. All rights reserved.
Tell Me What to Eat If I Have Acid Reflux Revised Edition
Nutrition You Can Live With
By Elaine Magee, Gina TalucciRed Wheel/Weiser, LLC
Copyright © 2009 Elaine Magee, MPH, RDAll rights reserved.
ISBN: 978-1-60163-019-3
Contents
Foreword,Introduction,
Publisher's Note,
Chapter 1: Everything You Ever Wanted to Ask Your Doctor About Acid Reflux,
Chapter 2: Everything You Ever Wanted to Know About Food and Acid Reflux,
Chapter 3: The 10 Food Steps to Freedom,
Chapter 4: Waiting to Lose Weight,
Chapter 5: How to Have a Heartburn-Free Holiday,
Chapter 6: Recipes You Can't Live Without,
Chapter 7: Restaurant Rules,
Index,
About the Author,
CHAPTER 1
Everything You Ever Wanted to Ask Your Doctor About Acid Reflux
True, the majority of the book is devoted to the lifestyle and diet treatment options for acid reflux. Don't worry, we'll get to that. Acid reflux is the best-known term for gastroesophageal reflux disease, otherwise known as GERD. For our discussion we will use the term acid reflux, but know that reflux can be made up of acid and nonacid reflux. But first, you need to understand the who, what, where, why, and how of acid reflux. What is acid reflux? How do I got relief from my symptoms? What are my medical options — from over-the-counter products to surgery — and what are their side effects and risks? Answering these questions is what this chapter is all about. It's about everything you ever wanted to ask your doctor about acid reflux — if you could ever have his or her undivided attention for about an hour or two.
Q: Who has acid reflux?
If you have acid reflux, you are definitely not alone. More than 15 million Americans suffer from heartburn daily (a major symptom of acid reflux), with an additional 45 million having heartburn at least once a month. Do the math. That quickly adds up to at least 10 percent of Americans having some degree of acid reflux disease.
Q: What's going on inside my body with acid reflux?
When you have acid reflux, acid from the stomach flows backward up into the esophagus. So the word acid comes from the stomach acid, and the word reflux comes from the "backward flow" (or refluxing) of this stomach acid into the lower esophagus. Sounds rather simple doesn't it? But this little backsplash of the stomach acid contents comprised of acid and nonacidic material can injure the lining of your esophagus and wreak havoc in your life. It can disturb sleep, make you very uncomfortable after meals, cause a great deal of pain and discomfort, and, when untreated, can lead to serious complications.
When the body is functioning normally, this backsplash of stomach acid should never even reach as far up as the esophagus. You see, our bodies have a muscular valve called the lower esophageal sphincter, which connects the lower end of the esophagus with the upper end of the stomach. Food is only supposed to flow downward from the esophagus into the stomach where the food proceeds to get digested. But with acid reflux disease, this valve relaxes too frequently and allows some stomach acid to flow backward up into the esophagus.
Q: Is there a cure for acid reflux?
Acid reflux is a recurrent and chronic disease that does not resolve itself and go away. Anyone who has suffered from it for many years can tell you that. But long-term medical and lifestyle therapy is usually effective; it helps relieve symptoms in most people. Treatment options include lifestyle changes, medications, surgery, or a combination of those options — most help to keep the stomach acid from entering the lower esophagus.
Q: What is the most common symptom?
Heartburn! Thirty to 45 minutes after a heavy meal, heartburn hits. When excessive amounts of acid reflux enter the lower esophagus, the biggest result is heartburn, which is described as a feeling of burning discomfort right behind the breastbone (or heart) area of the body, that moves up toward the neck and throat. The burning can last for several hours and is often the worst after meals. Having heartburn every now and then isn't necessarily acid reflux or a health "problem." But when heartburn is frequent (two or more times a week) or accompanied by other symptoms (food sticking in the throat, blood loss, or weight loss), that's when acid reflux becomes the diagnosis. Some people even taste the sour stomach acid in the back of the throat.
Q: What are the other symptoms of acid reflux?
Besides heartburn, other common symptoms of acid reflux can include:
• a sensation of food coming back into the mouth accompanied by an acidic or sour taste.
• hoarseness.
• chronic cough.
• chronic asthma.
• belching.
• bloating.
Q: What can I do for just occasional heartburn?
For occasional heartburn, many people have found relief by using over-the-counter medicines and making some changes in their food habits and lifestyle, which include:
• avoiding foods and beverages that may be contributing to heartburn (more on this in Chapter 2).
• quitting smoking.
• trimming off some extra pounds if you are overweight. (I know from personal experience — this is absolutely "easier said than done.") This is so important that Chapter 4 is entirely devoted to it.
• eating your last meal or snack three hours or more before you go to sleep. When you allot that much time, there is a better chance that you are going to sleep on a somewhat empty stomach. The contents of the stomach should be small, and therefore less likely to splash up into the esophagus when you lay down.
Q: Is heartburn just the result of bad habits or does it have a physical cause?
You may be able to point your finger at bad eating habits for "occasional" heartburn. Habits such as overeating during meals that are high in fat, over-indulging in alcohol, and eating certain irritating food products such as citrus juices, spicy tomato products, or chocolates, can cause heartburn — even in healthy individuals. But when you have more frequent heartburn and other symptoms of acid reflux, there is more likely a physical cause.
Q: What about pregnant women and heartburn?
For many women, their first introduction to heartburn is their last few months of pregnancy, but there is a good explanation for this. The growing baby presses on the stomach, which can cause backward flow of stomach contents into the esophagus. The bad news is this type of heartburn is often resistant to dietary changes and even antacids. The good news is, once the baby is born, the heartburn most often disappears.
Q: What is the key to relieving the symptoms?
If the physical cause of acid reflux is the stomach acid refluxing into the esophagus from the stomach, then suppressing that acid and keeping it from irritating esophageal tissue is the key in relieving the symptoms and letting the irritated tissue heal.
Q: When are symptoms the worst?
Esophageal acid exposure in people with esophagitis is typically more frequent during the day than at night, and especially after meals. Irritation and injury of esophageal tissue can take place directly after meals, because that's when acid is released from the stomach and the esophageal sphincter can have a tendency to relax, allowing the stomach acid to splash into the esophagus.
For others, heartburn tends to rear its ugly head at bedtime. That's when all the foods and beverages we probably shouldn't have had in excess come back and haunt us. When you lie down to go to sleep, you shift the stomach from an up-and-down position to a sideways position, and suddenly the opening to the esophagus is level with the rest of the stomach and its contents.
Q: What are my treatment options?
Acid reflux is usually treated with a combination of diet and lifestyle changes, over-the-counter or prescription medications, and in some cases, surgery. Most doctors start with the least invasive, least expensive options, such as over-the-counter medicines and changing some troublesome lifestyle habits, and then work their way to more intensive treatments, such as prescription medications and surgery.
Q: How is heartburn different from GERD/acid reflux?
Everyone experiences heartburn sometime in his or her life. But when the heartburn progresses from occasional heartburn to more than twice a week heartburn ... or the heartburn is associated with any of the various complications (such as food sticking, weight loss, low blood count), your heartburn has most likely developed into acid reflux disease.
Q: Which drugs are best for acid reflux and how do they work?
The following drugs offer effective treatment to "some" or "most" people. However, keep in mind that none of the current drugs used to treat acid reflux actually cures it. They help control symptoms and some also allow the esophagus to heal if there is tissue damage. Even when the drugs relieve symptoms completely, the condition usually reoccurs within months after the drugs are discontinued.
Q: What do over-the-counter antacids and foaming agents (alginic acid) do?
Antacids are great for rapidly relieving heartburn symptoms. They work directly in the stomach to decrease the acidity of the reflux liquid irritating the esophagus. They also help neutralize the area inside the esophagus. When antacids and a foaming agent are combined, they produce a foam barrier in the stomach, which floats over the contents of the stomach, preventing acid from splashing up into the esophagus. They do not heal esophagitis or prevent complications of acid reflux.
Q: What are the side effects of long-term use of antacids?
• Diarrhea from some antacids (Milk of Magnesia) and constipation from others (Amphogel, Alternagel). Aluminum and magnesium salts are used together in Mylanta and Maalox to help balance the side effects of diarrhea and constipation.
• Constipation can be caused by calcium carbonate (Tums, Titralac, and Alka-2). These over-the-counter antacids are a source of calcium, and in rare cases, can lead to too much calcium in the blood, leading to kidney failure.
• A change in the way the body breaks down and uses calcium.
• An increased risk of kidney stones.
• A buildup of magnesium in the body can be serious for patients with kidney disease.
If antacids are needed for more than three weeks, a doctor should be consulted.
Q: Can they interact with other drugs I might be taking?
Antacids can reduce the absorption of certain drugs (tetracycline, ciprofloxacin (Cipro), propanolol (Inderal), captopril (Capoten), and H2 blockers), so please let your doctor know if you are using antacids (even if you only use them every now and then). It will help to take the other drugs one hour before or three hours after you take the antacid.
Q: H2 blockers — what do they do?
H2 blockers (also called H2 receptor antagonists), help inhibit acid secretion in the stomach (which helps reduce the stomach acid that tends to worsen symptoms). Specifically, they work to block the type II histamine receptor that is one of the mechanisms controlling acid production. They work in about 30 minutes and last up to eight hours.
There are over-the-counter H2 blockers and prescription H2 blockers. The over-the-counter version does not relieve symptoms as quickly as antacids, but they last longer. In other words, they may be slow to start, but once they get going, they help your acid reflux for a long time.
H2 blockers have been the traditional drug treatment in acid reflux because many of them can be an effective short-term therapy for resistant acid reflux symptoms. In most studies on H2 blockers, where the participants were taking these drugs twice a day, symptoms were eliminated in up to half of the people. In one particular study (participants took ranitidine, 150 mg, twice a day), people were healed of their esophagitis within six weeks.
When taking these drugs keep three things in mind:
1. High doses are more effective than the more standard doses.
2. Taking them twice a day is more effective than taking them once a day.
3. H2 blockers are generally less expensive than proton pump inhibitors (see page 28 to find out more about proton pump inhibitors).
Over-the-counter version
A lower-dose, over-the-counter version of H2 blockers is available to help control "episodes" of heartburn, under the names cimetidine (100 mg), famotidine (10 mg), nizatidine (75 mg), and ranitidine (75 mg). They take longer to act than antacids (symptom relief may take 30 to 60 minutes), but they last longer.
You've probably seen these advertised on TV
Commercials abound for a couple of the drugs in this category. You know them by name — Tagamet HB, Pepcid AC, and Zantac 75.
For Tagamet (cimetidine), the prescribed dose is usually 300 mg, three times a day for four to six weeks, and many people experience improvement after two to four weeks. Because antacids reduce the absorption of Tagamet, make sure you take your antacids an hour before or after Tagamet is taken. Some take the H2 blocker before eating and antacids after eating.
For Zantac (ranitidine HCl), the prescribed dose is usually 150 mg two times a day for four to six weeks depending on the response. For people whose symptoms mainly appear at night, a single dose of 300 mg taken at bedtime might do the trick.
Warning: Even though these drugs are available without a prescription from your doctor, you should seek medical attention for persistent heartburn.
Side effects
These drugs, for the most part, have few side effects. Headache is the most common one cited. Other side effects reported are mild, temporary diarrhea, dizziness, and a rash; liver and nerve disease exacerbate these side effects. Another concern is that long-term acid suppression with these drugs may cause cancerous changes in the stomach in people who also have untreated H. pylori infections (this also goes for long-term use of proton pump inhibitor drugs).
• Tagamet (cimetidine) interacts with a number of common medications (phenytoin, theophylline, and wafarin). Long-term use of excessive doses (more than 3 g a day) of cimetidine may cause impotence or breast enlargement (these problems reverse after the drug is discontinued).
• Zantac (ranitidine) interferes with very few drugs.
• Axid (famotidine and nizatidine), the latest H2 blocker, is nearly free of side effects or drug interactions.
Promotility agents
These drugs are used for mild to moderate acid reflux symptoms and they are especially good at decreasing heartburn symptoms at night. They are often paired with H2 blockers to work together — they act in different ways to reduce symptoms. Although prescription H2 blockers moderately suppress acid, promotility agents:
• increase the strength of the lower esophageal sphincter muscle.
• speed up emptying of the stomach contents and enhance esophageal motility or movement through the esophagus. (Cisapride, bethanechol, erythromycin, and metoclopramide are the four promotility agents currently available.)
Side effects
Erythromycin is an antibiotic and can cause nausea and diarrhea.
Metoclopramide can include side effects such as drowsiness, anxiety, agitation, and motor restlessness in up to 30 percent of patients. The effect of this drug is more pronounced when given intravenously rather than orally.
Cisapride (Propulsid) should be avoided by people with certain disorders including, but not limited to, almost any heart disease, kidney failure, apnea, emphysema, chronic bronchitis, advanced cancer, and conditions that increase the risk for electrolyte disorders (imbalances in potassium, magnesium, sodium, or calcium). And it should be used with caution in people with liver disorders. The Food and Drug Administration states that Propulsid should not be used by people taking antiallergy, antiangina, and antiarrhythmics (irregular heart rhythm drugs) medicines, or antibiotics, antidepressants, antifungals, antinausea, antipsychotics, or protease inhibitors (for HIV). The FDA also advises that Propulsid should not be prescribed to anyone with a history of irregular heartbeats, abnormal electrocardiogram, heart disease, kidney disease, lung disease, eating disorder, dehydration, persistent vomiting, or low levels of potassium, calcium, or magnesium.
Proton pump inhibitors
Proton pump inhibitors claim that they heal erosive esophagitis more rapidly than H2 blockers. They do this by decreasing the acidity of the stomach contents by inhibiting an enzyme necessary for acid secretion.
Doctors are now using these as the mainstay for acid reflux treatment, because they provide potent acid suppression — a better way to help relieve symptoms and to let irritated tissues get a chance to heal more completely. These drugs may help control meal-stimulated acid secretion, but acid reflux during sleep can still occur with patients who are taking these drugs.
The proton pump inhibitor drugs available by prescription include omeprazole (Prilosec), esoemprazole (Nexium), lansoprazole (Prevacid), rabeprazole (Aciphex), pantoprazole (Protonix), and Zegerid (a newer combination of omeprazole and sodium bicarbonate). For the most part, they work similarly, and they are only used when symptoms are severe or when there is damage to the esophagus lining.
What they do
These drugs maintain a stomach acid level pH of more than 4.0. They do this by almost completely turning off the acid producing pumps of the stomach. In the right doses, proton pump inhibitor medications are the most effective agents for healing esophagitis and preventing complications (something the other drugs aren't as good at doing). They also provide a more complete rapid relief of acid reflux symptoms. With the exception of rabeprazole, which will have an onset of action in about 40 minutes, drugs of this class will take about two to six hours to begin having an effect of lowering acid production. After 24 hours they will have a more profound acid-lowering effect than any other class.
(Continues...)Excerpted from Tell Me What to Eat If I Have Acid Reflux Revised Edition by Elaine Magee, Gina Talucci. Copyright © 2009 Elaine Magee, MPH, RD. Excerpted by permission of Red Wheel/Weiser, LLC.
All rights reserved. No part of this excerpt may be reproduced or reprinted without permission in writing from the publisher.
Excerpts are provided by Dial-A-Book Inc. solely for the personal use of visitors to this web site.
- Mua astaxanthin uống có tốt không? Mua ở đâu? 29/10/2018
- Saffron (nhụy hoa nghệ tây) uống như thế nào cho hợp lý? 29/09/2018
- Saffron (nghệ tây) làm đẹp như thế nào? 28/09/2018
- Giải đáp những thắc mắc về viên uống sinh lý Fuji Sumo 14/09/2018
- Công dụng tuyệt vời từ tinh chất tỏi với sức khỏe 12/09/2018
- Mua collagen 82X chính hãng ở đâu? 26/07/2018
- NueGlow mua ở đâu giá chính hãng bao nhiêu? 04/07/2018
- Fucoidan Chính hãng Nhật Bản giá bao nhiêu? 18/05/2018
- Top 5 loại thuốc trị sẹo tốt nhất, hiệu quả với cả sẹo lâu năm 20/03/2018
- Footer chi tiết bài viết 09/03/2018
- Mã vạch không thể phân biệt hàng chính hãng hay hàng giả 10/05/2023
- Thuốc trắng da Ivory Caps chính hãng giá bao nhiêu? Mua ở đâu? 08/12/2022
- Nên thoa kem trắng da body vào lúc nào để đạt hiệu quả cao? 07/12/2022
- Tiêm trắng da toàn thân giá bao nhiêu? Có an toàn không? 06/12/2022
- Top 3 kem dưỡng trắng da được ưa chuộng nhất hiện nay 05/12/2022
- Uống vitamin C có trắng da không? Nên uống như thế nào? 03/12/2022
- [email protected]
- Hotline: 0909977247
- Hotline: 0908897041
- 8h - 17h Từ Thứ 2 - Thứ 7
Đăng ký nhận thông tin qua email để nhận được hàng triệu ưu đãi từ Muathuoctot.com
Tạp chí sức khỏe làm đẹp, Kem chống nắng nào tốt nhất hiện nay Thuoc giam can an toan hiện nay, thuoc collagen, thuoc Dong trung ha thao , thuoc giam can LIC, thuoc shark cartilage thuoc collagen youtheory dau ca omega 3 tot nhat, dong trung ha thao aloha cua my, kem tri seo hieu qua, C ollagen shiseido enriched, và collagen shiseido dạng viên , Collagen de happy ngăn chặn quá trình lão hóa, mua hang tren thuoc virility pills vp-rx tri roi loan cuong duong, vitamin e 400, dieu tri bang thuoc fucoidan, kem chống nhăn vùng mắt, dịch vụ giao hang nhanh nội thành, crest 3d white, fine pure collagen, nên mua collagen shiseido ở đâu, làm sáng mắt, dịch vụ cho thue kho lẻ tại tphcm, thực phẩm tăng cường sinh lý nam, thuoc prenatal bổ sung dinh dưỡng, kem đánh răng crest 3d white, hỗ trợ điều trị tim mạch, thuốc trắng da hiệu quả giúp phục hồi da. thuốc mọc tóc biotin
















 KHUYẾN MÃI LỚN
KHUYẾN MÃI LỚN Hỗ Trợ Xương Khớp
Hỗ Trợ Xương Khớp Bổ Não & Tăng cường Trí Nhớ
Bổ Não & Tăng cường Trí Nhớ Bổ Sung Collagen & Làm Đẹp
Bổ Sung Collagen & Làm Đẹp Bổ Thận, Mát Gan & Giải Độc
Bổ Thận, Mát Gan & Giải Độc Chăm Sóc Sức khỏe Nam Giới
Chăm Sóc Sức khỏe Nam Giới Chăm Sóc Sức khỏe Nữ Giới
Chăm Sóc Sức khỏe Nữ Giới Chăm sóc Sức khỏe Trẻ Em
Chăm sóc Sức khỏe Trẻ Em Thực Phẩm Giảm Cân, Ăn Kiêng
Thực Phẩm Giảm Cân, Ăn Kiêng Bổ Sung Vitamin & Khoáng Chất
Bổ Sung Vitamin & Khoáng Chất Bổ Tim Mạch, Huyết Áp & Mỡ Máu
Bổ Tim Mạch, Huyết Áp & Mỡ Máu Bổ Mắt & Tăng cường Thị lực
Bổ Mắt & Tăng cường Thị lực Điều Trị Tai Mũi Họng
Điều Trị Tai Mũi Họng Sức Khỏe Hệ Tiêu hóa
Sức Khỏe Hệ Tiêu hóa Chăm Sóc Răng Miệng
Chăm Sóc Răng Miệng Chống Oxy Hóa & Tảo Biển.
Chống Oxy Hóa & Tảo Biển.